What causes Endometriosis?
Posted by Rebecca
ENDOMETRIOSIS - Indescribable pain comparable with childbirth!
Why do I have endometriosis? What causes it? Why is it so painful? How do i treat it?
Unfortunately, endometriosis is a condition that comes with more questions than answers. March is endometriosis awareness month and support and information is always needed by this community of sufferers. Conventional medicine fails miserably in its handling of the condition in terms of both diagnosis and treatment. The problem with endometriosis is that there are many drivers behind it including: -
👉Hormonal - the balance between oestrogen and progesterone
👉Immune - Inflammation and gut bacteria, especially LPS endotoxins
👉Environmental toxins - Dioxins, plastics, pesticides etc.
How do I know I have Endometriosis?
Many women struggle for years to get a diagnosis for endometriosis. Common symptoms are: -
Heavy menstrual periods
Infertility
Tiredness
Digestive symptoms, constipation, bloating, nausea, IBS
Urinary tract issues
Other autoimmune conditions such as hashimoto's (underactive thyroid disease).
and PAIN, PAIN, PAIN!
Back Pain | Pelvic Pain | Pain during Sex | Pain with bowel movements or urinating | Period pain
If your period pain cannot be resolved with over the counter pain medication then this is not normal.
COMMON, BUT NOT NORMAL!
Women's pain is dismissed all to often with comments such as "its all in your head" and "just take a paracetamol" and my favourite, "well does it stop you from doing anything"!!
I believe one of the reasons why women are not taken seriously early enough is because in my experience, women can endure incredible stress in their lives and just find ways to carry on.
What is endometriosis and what causes it?
Endometriosis is the process of endometrial cells (usually found in the uterus) implanting in tissue and growing outside the uterus. Common locations include the pelvic cavity and reproductive organs. These cells form lesions and adhesions that can stick tissues of other organs together and cause immense pain. Active patches of lesions respond to our usual cyclical hormones and can produce their own localised oestrogen and inflammatory chemical messengers.
Why does this happen?
Retrograde menstruation is one theory, where the menstrual blood flows back through the uterus into and out of the fallopian tubes. However, this is common in many women and doesn't always result in the pain of endometriosis. Many women can live with endometriosis without ever knowing they have it.
Sound pretty unfair, so what happens in women that do have pain?
No-one knows the exact cause but key explanations are:-
Genetic predisposition
Hormonal imbalances (excess oestrogen)
Immune dysfuction
Environmental toxins, such as dioxins,
Conventional medicine predominantly addresses the hormonal aspect because oestrogen stimulates the growth of the lesions. Endometrial lesions create a viscous cycle in an oestrogenic environment that: -
produces more oestrogen that →produces inflammatory chemicals that in turn→ produces more oestrogen.
Shutting down our hormones, not only ignores the immune component but may not be an option for a large amount of younger women that want to get pregnant.
This blog focuses on the immune dysfunction and nutritional support that can alleviate symptoms. To read more about how to support oestrogen levels naturally read my blog on ostrogen.
Immune function, Inflammation and Gut health. What is the link?
In women that don't have endometriosis the immune system recognises endometrial cells that are not in the uterus and destroys them. In women with endometriosis, the immune system fails to destroy all the cells and trys to repair the lesions that then creates scar tissue.
Around 80% of women with endometriosis have irritable bowel syndrome (IBS). This is no coincidence as the health of our gut is linked to our immune function.
The bacterial environment in our gut is comprised of beneficial and pathogenic bacteria. If the balance is in favour of the pathogenic bacteria this is called dysbiosis. Key factors linked to poor gut health and an increase in pathogenic bacteria include: -
Long term medications – oral contraceptives, antibiotics etc.
Chronic stress
Poor diet – processed foods, alcohol and sugar
Common food sensitivities – gluten, dairy, nuts, eggs and soy
Parasites, bacterial infections and viruses.
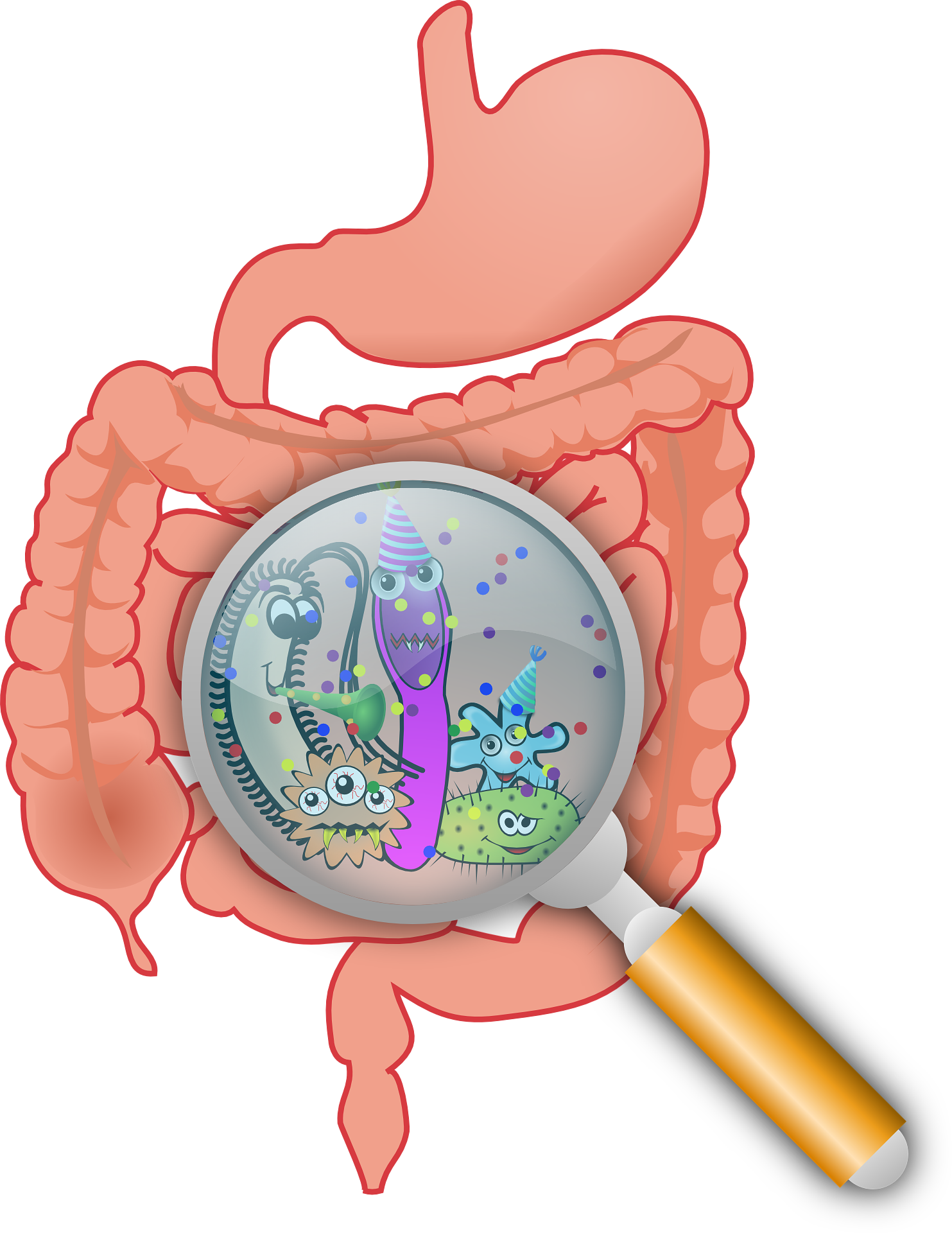
When our guts are unhealthy, the protective mucosal lining thins and the tight junctions loosen. This allows pathogenic bacteria to pass through the gut lining into systemic circulation. Gram-negative bacteria produce lipopolysaccharide (LPS) endotoxins that trigger a response from the immune system with the release of pro-inflammatory cytokines.
Over time our immune response becomes unreliable, which may lead to the development of autoimmune conditions. The immune response needs to be rebalanced and to do this the gut needs to be supported.
Nutrition and Immune function.
First, work with a nutritional therapist and check your gut health with a stool test. Functional testing companies offer comprhensive testing that report on various markers such as digestive health, bacterial balance, yeasts and parasites.
If pathogenic bacteria or parasites are an issue for you then there are many natural antimicrobials that your nutritionist can recommend.
Cut out food antigens, that means foods that are triggering your symptoms (both gut and endo symptoms). Common antigens are gluten, dairy and nuts.
Avoid alcohol. Sorry to say it but alcohol supports the transfer of LPS bacteria across the gut wall. We do not want them travelling to our pelvic area creating more inflammation and pain.
Support your beneficial bacteria by eating a diet high in fibre. Prebiotic foods that feed our beneficial bacteria include artichoke, leeks, asparagus, apples and onions.
Increase omega-3 fatty acids and healthy fats such as olive oil and avocado. They support the bodies production of anti-inflammatory chemical messengers (prostaglandins). Oily fish such as sardines, mackerel and wild salmon are excellent sources of omega-3.
Include anti-inflammatory foods such as ginger and turmeric in your diet.
Increase your intake of green leafy vegetables and cruciferous vegetables such as cauliflower and broccoli. They all contain numerous vitamins and minerals that support your liver in eliminating excess oestrogen.
Finally, address your stress levels.
Most of the women that I see in my clinic have stress as a major contributing factor to their illness. Make time for yourself a priority.
If you are struggling with your symptoms and need support putting the advice into practice, then book a discovery call with me to find out more about how I can help.
Tagged as: Endometriosis
Share this post: